Community
50 Events and Tours Featured in Bay Area Science Festival
By Kathleen Masterson, UCS News
Judy Sakanari’s lab receives and studies over a thousand worms a week. These aren’t your garden-variety slimers: her lab studies nematodes, flatworms and other parasites that cause debilitating diseases around the world. Some are so tiny you need a microscope to see them; they can enter human skin and worm their way into the brain.
Sakanari, PhD, is opening her lab for a public tour as a part of the Bay Area Science Festival (BASF) on Sunday, Oct. 26 at 2 p.m. The parasite lab tour is first come, first served, and it’s limited to 20 people total. It’s one of many free tours offered as a part of the festival’s Explorer Days.
The 10-day festival runs from Oct. 23 to Nov. 1 and includes over 50 events for families, adults and children, ranging from science storytelling competitions to concerts to interactive tours with scientists to lectures on current science topics. This year marks the 4th annual Bay Area Science Festival, which was created by the Bay Area’s scientific, cultural, and educational institutions, including Science & Health Education Partnership (SEP) at UCSF.
In a cramped, windowless room with a biohazard sign on the door, Sakanari pulls out a petri dish containing several reddish snails. These inconspicuous creatures are the host for part of a life cycle for the parasite Schistosoma, which causes Katayama fever and can lead to liver damage, kidney failure, and more.
After Sakanari warms the snails under a lamp to mimic sunshine, soon microscopic, wriggling larvae scoot across the water.
“This is one that causes over 200 million infections worldwide, so it’s a very prevalent infection and causes chronic disability,” said Sakanari. “For a lot of parasitic infections, the infection may not be fatal right away, but the parasite can cause chronic disease that makes people disabled for many years.”
Visitors to the lab can peer through the microscope to check out the wriggling larvae. Sakanari shows how the tiny parasitic larvae have evolved to seek out human hosts: she smudges a tiny bit of oil from her finger into a dish, then adds the water with larvae. They squirm over to the invisible smudge, seeking out the human lipids like a missile.
Next stop in the lab tour: the Worminator. This nondescript black box is helping the scientists to test the effectiveness of different drugs on various worms, including onchocerca worms that live in black flies and cause River Blindness.
This disease can cause intense itching, rashes, eye lesions, and ultimately can progress to blindness. The lab is also testing drugs on Brugia worms, which are transmitted by mosquitoes and cause elephantiasis, a painful disease that can cause enlargement of the legs and arms.
Sakanari’s lab tech Christina Bulman pulls out a plastic case with rows of circular wells, each containing a long slippery worm not much fatter than a human hair. She places the case inside the Worminator, and then an image of the squirming worms shows on the computer screen.
Using software written by Sakanari’s former student, Chris Marcellino, the Worminator actually measures the speed of the worms’ movement, and the researchers use this to test how effective various drugs are at slowing or killing the disease-causing worms.
Visitors to the parasite lab can see these and other microscopic monsters on the hour-long tour on Sunday. Adults and supervised children are welcome on the lab tour.
Packed with family, child and adult events, the Bay Area Science Festival runs from Oct. 23 to Nov. 1. For a festival calendar, go to www.bayareascience.org/schedule/2014-10/?PageSpeed=noscript
Alameda County
Seth Curry Makes Impressive Debut with the Golden State Warriors
Seth looked comfortable in his new uniform, seamlessly fitting into the Warriors’ offensive and defensive system. He finished the night with an impressive 14 points, becoming one of the team’s top scorers for the game. Seth’s points came in a variety of ways – floaters, spot-up three-pointers, mid-range jumpers, and a handful of aggressive drives that kept the Oklahoma City Thunder defense on its heels.

By Y’Anad Burrell
Tuesday night was anything but ordinary for fans in San Francisco as Seth Curry made his highly anticipated debut as a new member of the Golden State Warriors. Seth didn’t disappoint, delivering a performance that not only showcased his scoring ability but also demonstrated his added value to the team.
At 35, the 12-year NBA veteran on Monday signed a contract to play with the Warriors for the rest of the season.
Seth looked comfortable in his new uniform, seamlessly fitting into the Warriors’ offensive and defensive system. He finished the night with an impressive 14 points, becoming one of the team’s top scorers for the game. Seth’s points came in a variety of ways – floaters, spot-up three-pointers, mid-range jumpers, and a handful of aggressive drives that kept the Oklahoma City Thunder defense on its heels.
One of the most memorable moments of the evening came before Seth even scored his first points. As he checked into the game, the Chase Center erupted into applause, with fans rising to their feet to give the newest Warrior a standing ovation.
The crowd’s reaction was a testament not only to Seth’s reputation as a sharpshooter but also to the excitement he brings to the Warriors. It was clear that fans quickly embraced Seth as one of their own, eager to see what he could bring to the team’s championship aspirations.
Warriors’ superstar Steph Curry – Seth’s brother – did not play due to an injury. One could only imagine what it would be like if the Curry brothers were on the court together. Magic in the making.
Seth’s debut proved to be a turning point for the Warriors. Not only did he contribute on the scoreboard, but he also brought a sense of confidence and composure to the floor.
While their loss last night, OKC 124 – GSW 112, Seth’s impact was a game-changer and there’s more yet to come. Beyond statistics, it was clear that Seth’s presence elevated the team’s performance, giving the Warriors a new force as they look to make a deep playoff run.
#NNPA BlackPress
LIHEAP Funds Released After Weeks of Delay as States and the District Rush to Protect Households from the Cold
BLACKPRESSUSA NEWSWIRE — The federal government has released $3.6 billion in home heating assistance after a delay that left states preparing for the start of winter without the program’s annual funding.

By Stacy M. Brown
Black Press USA Senior National Correspondent
The federal government has released $3.6 billion in home heating assistance after a delay that left states preparing for the start of winter without the program’s annual funding. The Low-Income Home Energy Assistance Program, known as LIHEAP, helps eligible households pay heating and cooling bills. The release follows a shutdown that stretched 43 days and pushed agencies across the country to warn families of possible disruptions.
State officials in Minnesota, Kansas, New York, and Pennsylvania had already issued alerts that the delay could slow the processing of applications or force families to wait until December for help. In Pennsylvania, more than 300,000 households depend on the program each year. Minnesota officials noted that older adults, young children, and people with disabilities face the highest risk as temperatures fall.
The delay also raised concerns among advocates who track household debt tied to rising utility costs. National Energy Assistance Directors Association Executive Director Mark Wolfe said the funds were “essential and long overdue” and added that high arrearages and increased energy prices have strained families seeking help.
Some states faced additional pressure when other services were affected by the shutdown. According to data reviewed by national energy advocates, roughly 68 percent of LIHEAP households also receive nutrition assistance, and the freeze in multiple programs increased the financial burden on low-income residents. Wolfe said families were placed in “an even more precarious situation than usual” as the shutdown stretched into November.
In Maryland, lawmakers urged the Trump administration to release funds after the state recorded its first cold-related death of the season. The Maryland Department of Health reported that a man in his 30s was found outdoors in Frederick County when temperatures dropped. Last winter, the state documented 75 cold-related deaths, the highest number in five years. Rep Kweisi Mfume joined more than 100 House members calling for immediate federal action and said LIHEAP “is not a luxury” for the 100,000 Maryland households that rely on it. He added that seniors and veterans would be placed at risk if the program remained stalled.
Maryland Gov. Wes Moore used $10.1 million in state funds to keep benefits moving, but noted that states cannot routinely replace federal dollars. His administration said families that rely on medical equipment requiring electricity are particularly vulnerable.
The District of Columbia has already mapped out its FY26 LIHEAP structure in documents filed with the federal government. The District’s plan shows that heating assistance, cooling assistance, weatherization, and year-round crisis assistance operate from October 1 through September 30. The District allocates 50 percent of its LIHEAP funds to heating assistance, 10 percent to cooling, 13 percent to year-round crisis assistance, 15 percent to weatherization, and 10 percent to administrative costs. Two percent is used for services that help residents reduce energy needs, including education on reading utility bills and identifying energy waste.
The District’s plan lists a minimum LIHEAP benefit of $200 and a maximum of $1,800 for both heating and cooling assistance. Crisis benefits are provided separately and may reach up to $500 when needed to resolve an emergency. The plan states that a household is considered in crisis if it has been disconnected from energy service, if heating oil is at 5 percent or less of capacity, or if the household has at least $200 owed after the regular benefit is applied.
The District’s filing notes that LIHEAP staff conduct outreach through community meetings, senior housing sites, Advisory Neighborhood Commissions, social media, posters, and mass mailings. The plan confirms that LIHEAP applicants can apply in person, by mail, by email, or through a mobile-friendly online application and that physically disabled residents may request in-home visits.
As agencies nationwide begin distributing the newly released funds, states continue working through large volumes of applications. Wolfe said LIHEAP administrators “have been notified that the award letters have gone out and the states can begin to draw down the funds.”
#NNPA BlackPress
Seven Steps to Help Your Child Build Meaningful Connections
BLACKPRESSUSA NEWSWIRE — Swinging side by side with a friend on the playground. Sharing chalk over bright, colorful sidewalk drawings. Hiding behind a tree during a spirited game of hide-and-seek. These simple moments between children may seem small, but they matter more than we think

By Niyoka McCoy, Ed.D., Chief Learning Officer, Stride/K12
Swinging side by side with a friend on the playground. Sharing chalk over bright, colorful sidewalk drawings. Hiding behind a tree during a spirited game of hide-and-seek. These simple moments between children may seem small, but they matter more than we think: They lay the foundation for some of life’s most important skills.
Through everyday play, young children begin learning essential social and emotional skills like sharing, resolving conflicts, showing empathy, and managing their emotions. These social skills help shape emotional growth and set kids up for long-term success. Socialization in early childhood isn’t just a “nice-to-have”—it’s essential for development.
Yet today, many young children who haven’t yet started school aren’t getting enough consistent, meaningful interaction with peers. Research shows that there’s a decline in active free play and peer socialization when compared to previous generations.
There are many reasons for this. Children who are home with a parent during the day may spend most of their time with adults, limiting opportunities for peer play. Those in daycare or preschool may have restricted free play, and large classrooms can reduce supervision and social coaching. Some children live in rural areas, are homebound due to illness, have full schedules, or rely on screens to fill their playtime. And for some families, finding other families with young children to connect with isn’t easy.
While these challenges can feel significant, opportunities for connection still exist in every community. Families can take simple steps to help children build friendships, create a sense of belonging, and strengthen social skills. Here are some ideas to get started:
- Storytime sessions at libraries or local bookstores
- Community offerings such as parent-child workshops, art, music, gymnastics, swimming, or sports programs
- Weekly events at children’s museums, which may include art projects, music workshops, or science experiments
- Outdoor exploration, where kids can play with peers
- Local parenting groups that organize playdates and group activities
- Volunteer opportunities where children can participate, such as pet adoption events or packing meals at a food bank
- Classes for kids at local businesses, including hardware, grocery, or craft stores
Some of these community activities are free or low-cost and give kids the chance to build friendships and practice social skills. Parents can also model positive social behavior by interacting with other parents and encouraging their children to play with their peers.
These may seem like small moments of connection, but they can have a powerful impact. Every time your child shares a toy, plays make-believe with peers, or races a friend down the slide, they’re not just playing—they’re learning the skills that build confidence, empathy, and lasting friendships. And it’s good for you, too. Creating intentional opportunities for play also helps you strengthen your own network of parents who can support one another as your children grow together.
-
 Activism3 weeks ago
Activism3 weeks agoOakland Post: Week of November 12 – 18, 2025
-

 Activism3 weeks ago
Activism3 weeks agoIN MEMORIAM: William ‘Bill’ Patterson, 94
-

 Activism3 weeks ago
Activism3 weeks agoHow Charles R. Drew University Navigated More Than $20 Million in Fed Cuts – Still Prioritizing Students and Community Health
-

 Bay Area3 weeks ago
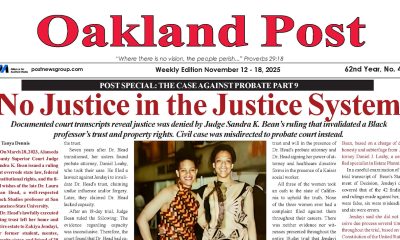
Bay Area3 weeks agoNo Justice in the Justice System
-

 #NNPA BlackPress2 weeks ago
#NNPA BlackPress2 weeks agoLewis Hamilton set to start LAST in Saturday Night’s Las Vegas Grand Prix
-

 #NNPA BlackPress3 weeks ago
#NNPA BlackPress3 weeks agoThe Perfumed Hand of Hypocrisy: Trump Hosted Former Terror Suspect While America Condemns a Muslim Mayor
-

 #NNPA BlackPress2 weeks ago
#NNPA BlackPress2 weeks agoBeyoncé and Jay-Z make rare public appearance with Lewis Hamilton at Las Vegas Grand Prix
-

 #NNPA BlackPress3 weeks ago
#NNPA BlackPress3 weeks agoTrump’s Death Threat Rhetoric Sends Nation into Crisis