Health
Report Urges Major Steps to Help Victims of Cardiac Arrest

LAURAN NEERGAARD, AP Medical Writer
WASHINGTON (AP) — Would you know what to do if you see someone collapse, not breathing — a loved one at home, a co-worker at the office, a stranger on the street? Far too many Americans die of cardiac arrest, and now a major new report urges a national campaign to improve survival in part by making sure more bystanders know how to help.
Every year, about 395,000 people suffer cardiac arrest in their homes or other non-hospital settings — and less than 6 percent of them survive, the Institute of Medicine estimated Tuesday.
That’s not the whole toll: An additional 200,000 cardiac arrests occur in hospitals every year, and even there only a quarter of patients survive, the report found.
Cardiac arrest is not a heart attack — it’s worse. It means the heart abruptly stops beating, its electrical activity knocked out of rhythm. CPR can buy critical time if it’s started immediately, but Tuesday’s report concludes the nation must take key steps to give victims a better shot.
“Cardiac arrest survival rates are unacceptably low,” said Dr. Robert Graham of George Washington University, who chaired the IOM committee’s investigation. “There is a lot an individual can do to assist somebody if they witness one, and to work with their communities to improve the system of response.”
What to do may sound straightforward: Call 911, and then start quick, hard compressions of the person’s chest until trained responders arrive. If a device called an AED — an automated external defibrillator — is available, use it.
In reality, the IOM committee said fear, not understanding what cardiac arrest is, lack of first-aid training and concern about legal liability can hamper response and cost precious time. Each year, less than 3 percent of the U.S. population receives training in CPR or defibrillator use, while some European countries mandate training, the report found.
Moreover, there are wide disparities in outcomes: One study found that survival ranged from about 8 percent to 40 percent across 10 different communities.
On Tuesday, the IOM called for a major public education effort to teach people how to recognize and react to cardiac arrest — including making CPR training a graduation requirement for high school. According to the American Heart Association, Connecticut just became the 24th state to pass legislation to do that.
State and local health departments should team with health groups to create “a culture of action,” the IOM recommended. It also urged employers to stock defibrillators and train workers to use them, and expanded access to CPR training for people over age 65 and their caregivers.
Good Samaritan laws provide varying legal protection by state. At the same time, laymen shouldn’t feel they have to provide perfect care, said IOM committee member Dr. Tom Aufderheide of the Medical College of Wisconsin.
“Any CPR and any early defibrillation delivered by the public is better than no care at all,” he said.
Other recommendations:
—The Centers for Disease Control and Prevention should create a national registry of cardiac arrest. There are no good statistics on this killer, the IOM said, calling its own numbers the best available estimates. A registry would track outcomes so communities could take steps to improve. The CDC said it will review the recommendation.
—National standards are needed for emergency medical systems, to ensure that 911 callers are talked through how to provide CPR.
—The National Institutes of Health should expand research for better treatments. Defibrillators attempt to shock the heart back into rhythm so it can resume beating, but most out-of-hospital cardiac arrests aren’t the kind of abnormal rhythms that a shock can fix, said IOM committee member Dr. Lance Becker of the University of Pennsylvania. Yet the report found the NIH spends far less on cardiac arrest research than on other cardiovascular problems.
—Hospitals should have to meet national accreditation standards on cardiac arrest care. Survival of patients who suffer cardiac arrest while hospitalized for some other reason can vary by 10 percent between hospitals, IOM found.
Improvement is possible, the IOM found, calling some communities examples. In King County, Washington, there’s a 62 percent survival rate among patients with a specific shockable form of cardiac arrest if they collapse in front of someone. Policymakers there have spent decades studying what care works best, and getting bystanders and professionals on board with response practices.
The American Heart Association — which along with the American Red Cross, American College of Cardiology and the federal government had requested the IOM’s study — welcomed the recommendations.
Cardiac arrest is “the most critically ill state a human being can be in,” said Dr. Robert W. Neumar of the University of Michigan, who chairs a heart association emergency care committee. The nation needs to create a culture where “if someone collapses in front of you with cardiac arrest, it’s your obligation to help.”
Copyright 2015 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
Advice
BOOK REVIEW: Let Me Be Real With You
At first look, this book might seem like just any other self-help offering. It’s inspirational for casual reader and business reader, both, just like most books in this genre. Dig a little deeper, though, and you’ll spot what makes “Let Me Be Real With You” stand out.
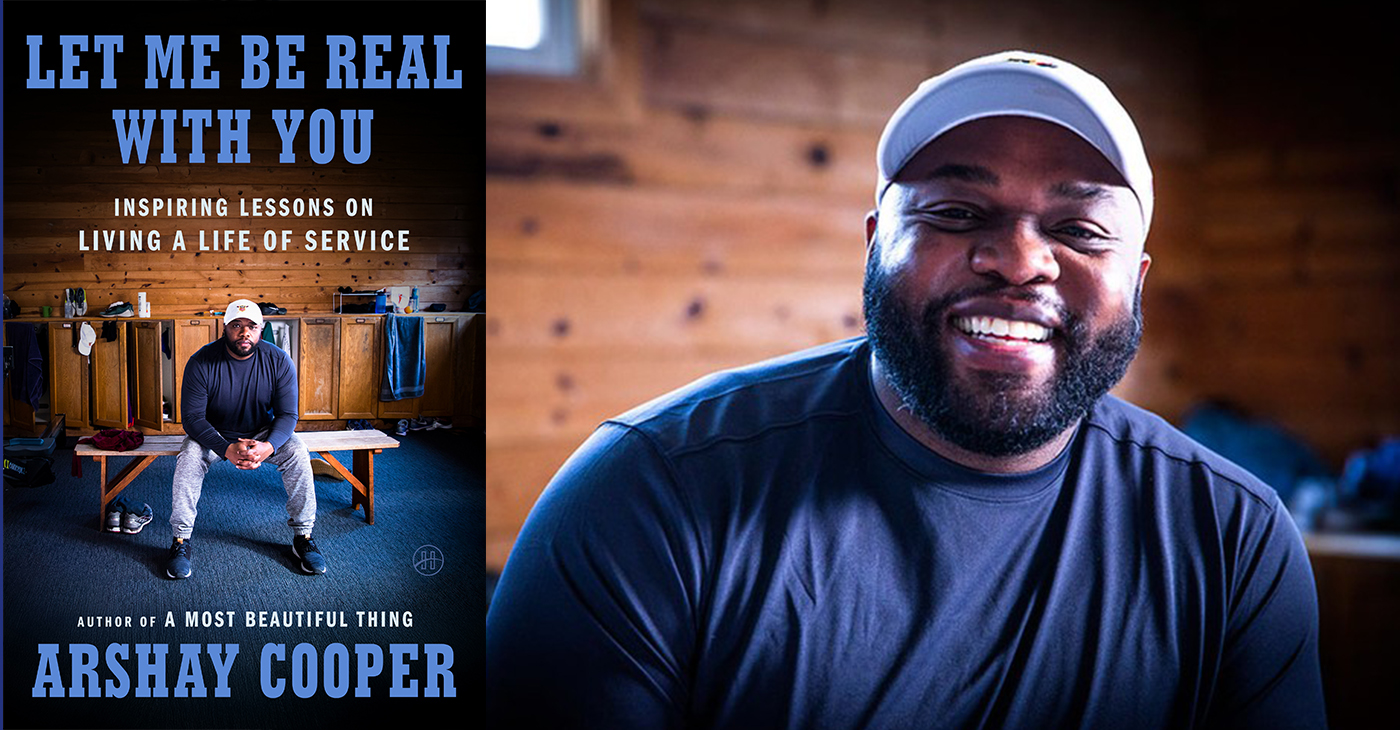
By Terri Schlichenmeyer
Author: Arshay Cooper, Copyright: c.2025, Publisher: HarperOne, SRP: $26.00, Page Count: 40 Pages
The hole you’re in is a deep one.
You can see the clouds above, and they look like a storm; you sense the wind, and it’s cold. It’s dark down there, and lonesome, too. You feel like you were born there — but how do you get out of the deep hole you’re in? You read the new book “Let Me Be Real With You” by Arshay Cooper. You find a hand-up and bring someone with you.
In the months after his first book was published, Cooper received a lot of requests to speak to youth about his life growing up on the West Side of Chicago, his struggles, and his many accomplishments. He was poor, bullied, and belittled, but he knew that if he could escape those things, he would succeed. He focused on doing what was best, and right. He looked for mentors and strove to understand when opportunities presented themselves.
Still, his early life left him with trauma. Here, he shows how it’s overcome-able.
We must always have hope, Cooper says, but hope is “merely the catalyst for action. The hope we receive must transform into the hope we give.”
Learn to tell your own story, as honestly as you know it. Be open to suggestions, and don’t dismiss them without great thought. Know that masculinity doesn’t equal stoicism; we are hard-wired to need other people, and sharing “pain and relatability can dissipate shame and foster empathy in powerful ways.”
Remember that trauma is intergenerational, and it can be passed down from parent to child. Let your mentors see your potential. Get therapy, if you need it; there’s no shame in it, and it will help, if you learn to trust it. Enjoy the outdoors when you can. Learn self-control. Give back to your community. Respect your financial wellness. Embrace your intelligence. Pick your friends and relationships wisely. “Do it afraid.”
And finally, remember that “You were born to soar to great heights and rule the sky.”
You just needed someone to tell you that.
At first look, this book might seem like just any other self-help offering. It’s inspirational for casual reader and business reader, both, just like most books in this genre. Dig a little deeper, though, and you’ll spot what makes “Let Me Be Real With You” stand out.
With a willingness to discuss the struggles he tackled in the past, Cooper writes with a solidly honest voice that’s exceptionally believable, and not one bit dramatic. You won’t find unnecessarily embellished stories or tall tales here, either; Cooper instead uses his real experiences to help readers understand that there are few things that are truly insurmountable. He then explains how one’s past can shape one’s future, and how today’s actions can change the future of the world.
“Let Me Be Real With You” is full of motivation, and instruction that’s do-able for adults and teens. If you need that, or if you’ve vowed to do better this coming year, it might help make you whole.
Advice
Support Your Child’s Mental Health: Medi-Cal Covers Therapy, Medication, and More

Advertorial
When children struggle emotionally, it can affect every part of their lives — at home, in school, with friends, and even their physical health. In many Black families, we’re taught to be strong and push through. But our kids don’t have to struggle alone. Medi-Cal provides mental health care for children and youth, with no referral or diagnosis required.
Through California Advancing and Innovating Medi-Cal (CalAIM), the state is transforming how care is delivered. Services are now easier to access and better connected across mental health, physical health, and family support systems. CalAIM brings care into schools, homes, and communities, removing barriers and helping children get support early, before challenges escalate.
Help is Available, and it’s Covered
Under Medi-Cal, every child and teen under age 19 has the right to mental health care. This includes screenings, therapy, medication support, crisis stabilization, and help coordinating services. Parents, caregivers, and children age 12 or older can request a screening at any time, with no diagnosis or referral required.
Medi-Cal’s Mental Health and Substance Use Disorder Program
For children and youth with more serious mental health needs, including those in foster care or involved in the justice system, Medi-Cal offers expanded support, including:
- Family-centered and community-based therapy to address trauma, behavior challenges, or system involvement.
- Wraparound care teams that help keep children safely at home or with relatives.
- Activity funds that support healing through sports, art, music, and therapeutic camps.
- Initial joint behavioral health visits, where a mental health provider and child welfare worker meet with the family early in a case.
- Child welfare liaisons in Medi-Cal health plans who help caregivers and social workers get services for children faster
Keeping Kids Safe from Opioids and Harmful Drugs
DHCS is also working to keep young people safe as California faces rising risks from opioids and counterfeit pills. Programs like Elevate Youth California and Friday Night Live give teens mentorship, leadership opportunities, and positive outlets that strengthen mental well-being.
Through the California Youth Opioid Response, families can learn how to avoid dangerous substances and get treatment when needed. Song for Charlie provides parents and teens with facts and tools to talk honestly about mental health and counterfeit pills.
DHCS also supports groups like Young People in Recovery, which helps youth build skills for long-term healing, and the Youth Peer Mentor Program, which trains teens with lived experience to support others. These efforts are part of California’s strategy to protect young people, prevent overdoses, and help them make healthier choices.
Support for Parents and Caregivers
Children thrive when their caregivers are supported. Through CalAIM’s vision of whole-person care, Medi-Cal now covers dyadic services, visits where a child and caregiver meet together with a provider to strengthen bonding, manage stress, and address behavior challenges.
These visits may include screening the caregiver for depression or anxiety and connecting them to food, housing, or other health-related social needs, aligning with CalAIM’s Community Supports framework. Notably, only the child must be enrolled in Medi-Cal to receive dyadic care.
Family therapy is also covered and can take place in clinics, schools, homes, or via telehealth, reflecting CalAIM’s commitment to flexible, community-based care delivery.
Additionally, BrightLife Kids offers free tools, resources, and virtual coaching for caregivers and children ages 0–12. Families can sign up online or through the BrightLife Kids app. No insurance, diagnosis, or referral is required.
For teens and young adults ages 13–25, California offers Soluna, a free mental health app where young people can chat with coaches, learn coping skills, journal, or join supportive community circles. Soluna is free, confidential, available in app stores, and does not require insurance.
CalHOPE also provides free emotional support to all Californians through a 24/7 support line at (833) 317-HOPE (4673), online chat, and culturally responsive resources.
Support at School — Where Kids Already Are
Schools are often the first place where emotional stress is noticed. Through the Children and Youth Behavioral Health Initiative (CYBHI), public schools, community colleges, and universities can offer therapy, counseling, crisis support, and referrals at no cost to families.
Services are available during school breaks and delivered on campus, by phone or video, or at community sites. There are no copayments, deductibles, or bills.
Medi-Cal Still Covers Everyday Care
Medi-Cal continues to cover everyday mental health care, including therapy for stress, anxiety, depression, or trauma; medication support; crisis stabilization; hospital care when needed; and referrals to community programs through county mental health plans and Medi-Cal health plans.
How to Get Help
- Talk to your child’s teacher, school counselor, or doctor.
- In Alameda County call 510-272-3663 or the toll-free number 1-800-698-1118 and in San Francisco call 855-355-5757 to contact your county mental health plan to request an assessment or services.
- If your child is not enrolled in Medi-Cal, you can apply at com or my.medi-cal.ca.gov.
- In a mental health emergency, call or text 988, the Suicide and Crisis Lifeline.
Every child deserves to grow up healthy and supported. Medi-Cal is working to transform care so it’s accessible, equitable, and responsive to the needs of every family.
Activism
ESSAY: The Hidden Toll — Federal Rollbacks Threaten Black Women’s Health in California
Nutrition assistance programs, which many Black women rely on to keep their families healthy and out of the hospital, are similarly endangered. Nearly half of Black women in California receive WIC, and 47% percent use CalFresh. Cuts or cost-shifts in those programs would worsen food insecurity, especially during pregnancy and postpartum. Malnutrition or diet instability can lead to adverse birth outcomes, weakened immunity, and worse recovery from medical interventions.

By Kellie Todd Griffin, Special to California Black Media Partners
If recent proposals in Congress to cut funding for federal social programs succeed, the downstream effects will not be abstract or distant.
They will be immediate and blunt — and felt in every clinic, every hospital, and most homes where Black women are struggling to maintain our health, care for her children, and stay afloat. In California, where Black women already navigate a terrain of deep systemic inequities, these cuts would be catastrophic.
As a lifelong advocate for Black women in California — through my research and lived experience – I’ve seen firsthand the entrenched medical and social disparities that leave too many Black women struggling to live healthy, fulfilling lives.
Across the spectrum of care — from mental, maternal, and perinatal health to chronic diseases like diabetes, hypertension, cancer, and uterine fibroids — Black women in California continue to bear a disproportionate burden.
Implicit bias in maternity care, for example, continues to be a challenge. It is a documented contributor to the fact that, in California, Black women die from pregnancy-related causes at three to four times the rate of White women.
Now, federal proposals on the table to slash funding for the very programs Black women rely on most: Medicaid (Medi-Cal in California) SNAP/CalFresh, WIC, and federal housing and income supports. As reported in the California Budget and Policy Equity on the Line report, about one in three Black women and children in California currently depend on Medi-Cal. If federal cuts were to force reductions in eligibility, benefits, or provider reimbursements, many Black women would lose access to primary care, chronic disease management, reproductive care, mental health and substance-use treatment, cancer screenings, and prenatal/postnatal services.
In a state already grappling with stark racial health disparities, removing coverage is not just harmful — it magnifies injustice. Black women in California face higher rates of poor health overall, lower life expectancy, and worse prenatal care statistics. When the safety net frays, they will be forced into impossible trade-offs: skip medications, delay care, or incur medical debt.
Nutrition assistance programs, which many Black women rely on to keep their families healthy and out of the hospital, are similarly endangered. Nearly half of Black women in California receive WIC, and 47% percent use CalFresh. Cuts or cost-shifts in those programs would worsen food insecurity, especially during pregnancy and postpartum. Malnutrition or diet instability can lead to adverse birth outcomes, weakened immunity, and worse recovery from medical interventions.
Compounding the harm is the assault on social determinants of health. The Equity on the Line analysis shows that housing assistance, income support, and childcare subsidies are already stretched thin. Any rollback will accelerate housing instability, homelessness risk, and family stress — all of which manifest in worse health outcomes: higher hypertension, depression, chronic illness, and reduced ability to adhere to medical regimens.
California has taken important steps to protect Black women’s health. One good example is Assembly Bill, AB 2319, authored by Assemblymember Lori D. Wilson (D-Suisun City). That law strengthens the Dignity in Pregnancy and Childbirth Act by expanding and enforcing implicit bias training for providers in perinatal settings, and requiring reporting and penalties for noncompliance.
The state is also taking legal and policy action to mitigate the impact of cuts to SNAP/CalFresh food stamp benefits – like mobilizing $80 million in state funds to support food banks. It is also taking action to shore up against federal cuts to Medi-Cal.
In our communities, organizations like California Black Women’s Health Project and Black Women for Wellness are already doing the groundwork — advocating for culturally centered care, education, and infrastructure to mitigate harm.
As Californians, we must all roll up our sleeves and amplify and bolster their efforts. These organizations serve as our voice. They are our watchdogs, too, documenting where bias persists, where systems fail, and where state enforcement is weak.
The stakes are too high for complacency. As we strategize to keep Black women healthy, we must also document and share our stories with others — every death, every untreated illness, every delayed pregnancy.
Let us be resolute, organized, hopeful, and persistent. California can be a model of how a state defends Black women’s health amid significant challenges, presenting a full vision to America, and the world, of how we can make health justice a reality and make California healthier for all our communities.
About the Author
Kellie Todd Griffin, President and CEO of the California Black Women’s Collective Empowerment Institute. With a deep commitment to equity and justice, she champions initiatives that amplify the voices and influence of Black women across California. Known for her strategic insight and passion for community empowerment, Kellie is a driving force in fostering systemic change and collective progress.
-

 Activism4 weeks ago
Activism4 weeks agoDesmond Gumbs — Visionary Founder, Mentor, and Builder of Opportunity
-

 Activism4 weeks ago
Activism4 weeks agoFamilies Across the U.S. Are Facing an ‘Affordability Crisis,’ Says United Way Bay Area
-

 Alameda County3 weeks ago
Alameda County3 weeks agoOakland Council Expands Citywide Security Cameras Despite Major Opposition
-

 Alameda County3 weeks ago
Alameda County3 weeks agoBling It On: Holiday Lights Brighten Dark Nights All Around the Bay
-

 Activism4 weeks ago
Activism4 weeks agoBlack Arts Movement Business District Named New Cultural District in California
-
 Activism4 weeks ago
Activism4 weeks agoLu Lu’s House is Not Just Toying Around with the Community
-

 Activism4 weeks ago
Activism4 weeks agoOakland Post: Week of December 17 – 23, 2025
-

 Activism2 weeks ago
Activism2 weeks agoFirst 5 Alameda County Distributes Over $8 Million in First Wave of Critical Relief Funds for Historically Underpaid Caregivers